BRAIN WITH PING PONG BALLS
INTERESTING TO KNOW:
RASMUSSEN'S ENCEPHALITIS
CAUSES:
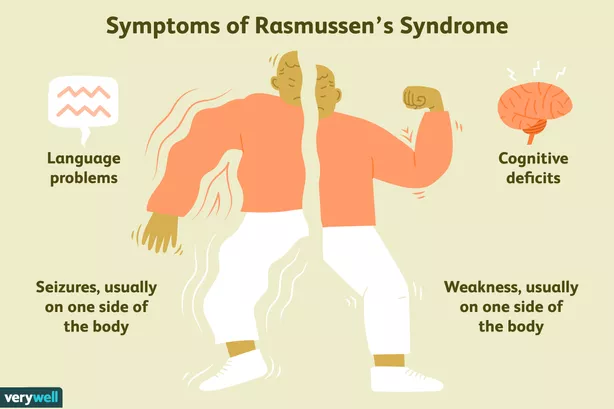
SYMPTOMS:
DIAGNOSIS:
TREATMENT:
HEMISPHERECTOMY
There are 2 main types of hemispherectomies: anatomic and functional.
- An anatomic hemispherectomy involves physically removing the diseased hemisphere of the brain including the frontal, parietal, temporal, and occipital lobes.
- A functional hemispherectomy is an evolution of the anatomic hemispherectomy in which less brain is removed, however, the diseased hemisphere of the brain is completely disconnected from the normal hemisphere of the brain.
INDICATIONS:
Hemispherectomy is indicated in patients with medically intractable epilepsy due to unilateral hemispheric lesions. Among them are included congenital (extensive, plurilobar cortical dysplasia, hemimegalencephaly, congenital extensive porencephaly, and SturgeWeber syndrome), and perinatal disorders (middle cerebral artery extensive infarcts, perinatal occlusion of the Sylvian aqueduct, Rasmussen encephalitis, West syndrome, and Lennox-Gastaut syndrome).
ANAESTHESIA:
The procedure is always performed under general endotracheal anesthesia and invasive cardiopulmonary monitoring (central venous line, intra-arterial line, transurethral catheter insertion). Warm air-blanket and intravenous fluids are essential for preventing perioperative hypothermia. A loading dose of steroids (dexamethasone) may be given intravenously in the morning of the surgery. Antibiotics, a gastro-protective agent, and anti-epileptic treatment are also indicated.
THE PROCEDURE:
The patient is positioned supine with a small shoulder bump and the head turned to the contralateral side.
Neuronavigation is very useful for confirming anatomical landmarks and ensuring that the midline is not breached during corpus callosotomy.
A skin incision should permit sufficient exposure of the working window. It is of importance to minimize bleeding with the use of Raney clips and bipolar cautery, especially in children. The skin-flap is elevated and reflected anteriorly. The underlying temporalis fascia is reflected anteriorly.
The underlying dura is detached from the bone with a #3 Penfield dissector. The adjacent burr holes are connected with a craniotome and the bone flap is carefully removed.
The dura is opened anteriorly, inferiorly, and posteriorly. Dural incision bleeding is controlled with hemostatic clips. The dural flaps, based toward the midline, are reflected.
- Anatomical hemispherectomy (AH) is performed under the surgical microscope and achieved in three phases. Initially, the Sylvian fissure is opened.
- In the second step, the corpus callosum is properly identified and divided through an interhemispheric approach.
- Finally, the fronto-basal white matter is divided through the anterior part of the lateral ventricle. The temporal stem is dissected and the ipsilateral anterior choroid and posterior communicating arteries are identified. The latter is clipped and divided at its P3 segment. The amygdala and the hippocampus are removed employing sub-pial dissection with special care on the preservation of the occulomotor nerve.
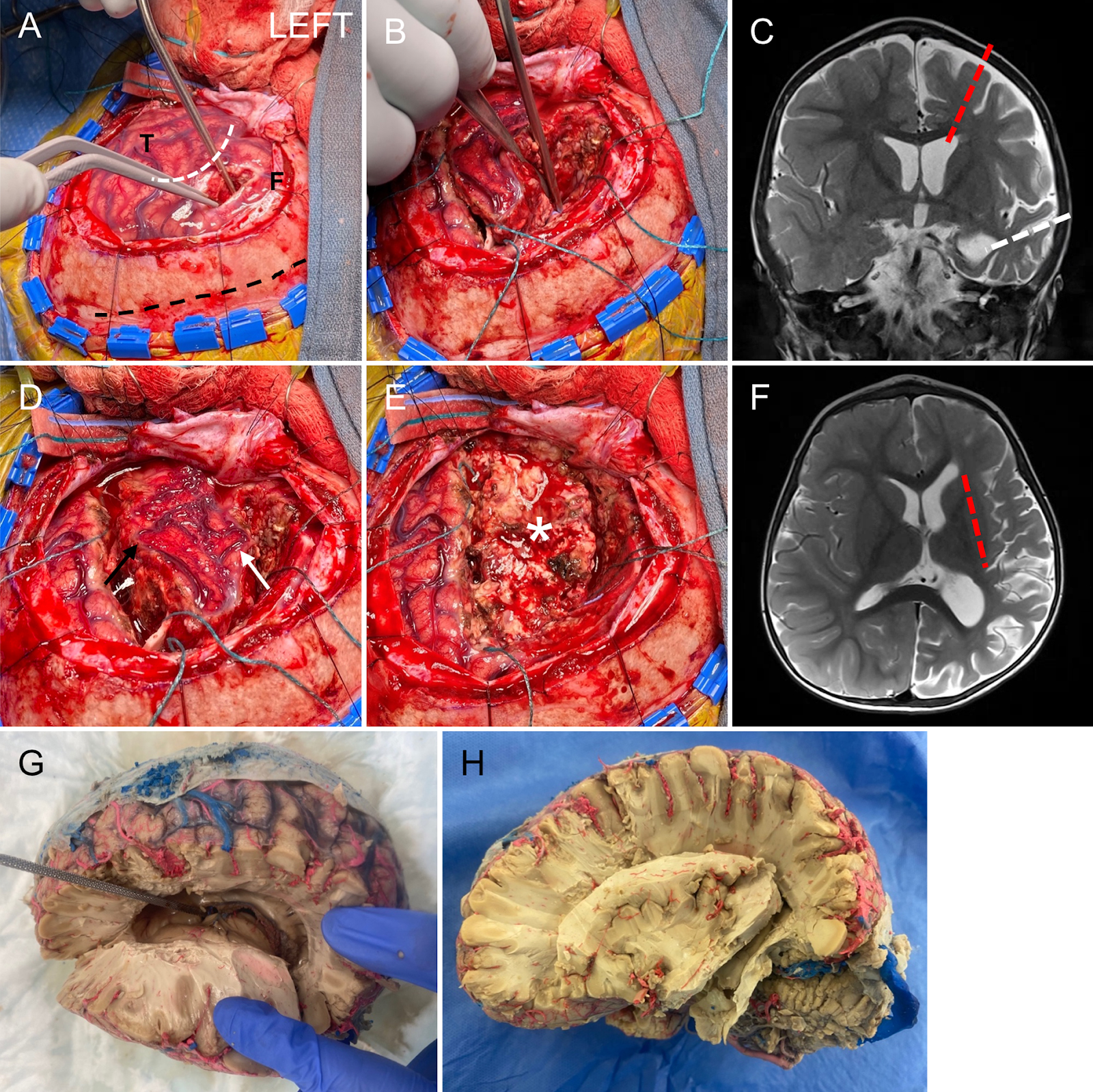
- Lateral disconnection. A: To disconnect the fibers forming the internal capsule and corona radiata, a cortisectomy is performed in the middle frontal gyrus into the frontal lateral horn of the lateral ventricle. The locations of the frontal lobe (F), temporal lobe (T), sylvian fissure (white dotted line), and midline (black dotted line) are shown. B: The cortisectomy is extended posteriorly to the supramarginal gyrus following the course of the lateral ventricle into the atrium and turns inferiorly toward the temporal horn. C: Coronal MR image showing the locations of the frontal (red dotted line) and temporal (white dotted line) cortisectomies. D: To facilitate surgical access, the frontal (white arrow) and temporal (black arrow) opercula are resected to expose the insula. E: The insular cortex is resected in a plane, which preserves the basal ganglia structures (asterisk). F: Axial MR image showing the location of the insular resection (red dotted line). G: Cadaveric specimen showing cortisectomy and exposure of the lateral ventricle anteriorly and posteriorly. The dissector is passed through the foramen of Monro. H: Cadaveric specimen showing removal of the opercula and insula.
Functional hemispherectomy (FH) is a four-step process.
- The temporal lobe is removed with two cortical incisions, one on the superior temporal gyrus, running in parallel to the Sylvian fissure, and a second one placed on the dorsal temporal lobe, down to the temporal base, perpendicular to the first one.
- The second step involves removal of the suprasylvian cortex by two parallel incisions perpendicular to the sylvian fissure, and providing access into the ipsilateral lateral ventricle.
- Completion of the transventricular parasagittal callosotomy is the main task of the third step.
- The remaining anterior and posterior callosal fiber tracts are disconnected from the ependymal surface toward the cingulate gyrus. Lastly, anterior and posterior disconnections of the frontal and parieto-occipital lobes take place.
- Mesial temporal resection. A: The temporal horn of the left lateral ventricle is opened to reveal the hippocampus (asterisk) and mesial structures. B: The anterior temporal lobe is resected, paying careful attention to the medial pial plane. When resection is complete, the oculomotor nerve is visualized on the other side of the pia (green arrow). C: Coronal MR image showing the temporal resection (red dotted line) and the relative position of the oculomotor nerve (green dot). D: Cadaveric specimen demonstrating the operative anatomy in panel A. The temporal horn is retracted to show the hippocampus (asterisk). The inferior choroidal point (black arrow) and the MCA bifurcation (limen insulae; yellow arrow) are connected and represent the medial extent of the amygdalectomy (red dotted line). E: The cadaveric specimen is reoriented to show the anatomical position of the hippocampus (asterisk), inferior choroidal point (black arrow), and MCA bifurcation (yellow arrow). TF = temporal floor; TP = temporal pole.
- Corpus callosotomy and completion of disconnections. A and B: Sagittal (A) and coronal (B) MR images showing the corpus callosotomy. The septum pellucidum is identified in the lateral ventricles, and the callosotomy is commenced millimeters lateral to the midline (red dotted lines). Anatomically, pericallosal branches of the ACA and the falx serve as landmarks (white arrow). The callosotomy is taken posteriorly through the body to the splenium until the atrium and the tentorial edge are reached (green dotted arrow). Anteriorly, the dissection follows the ACAs past the genu of the corpus callosum and courses inferiorly and posteriorly through the rostrum (yellow dotted arrow). C and D: Intraoperative views of the transventricular callostomy. The pericallosal ACA is outlined (white dotted line). CC = corpus callosum; S = midline septum. E and F: Anteriorly, the dissection through the rostrum of the corpus callosum is taken medially to the interhemispheric fissure and inferiorly to the anterior skull base. The frontobasal disconnection is completed, and the A1–2 junction serves as the posterior limit of the dissection (tip of the Penfield dissector). The dotted lines and white arrow in panel E denote the region of interest and direction of view, respectively, in panel F. G: Cadaveric specimen showing the transventricular corpus callostomy and ACA. H: Completion of the frontobasal (white arrow) and the parietooccipital (black arrow) disconnections. The basal ganglia and thalamus have been removed to aid anatomical visualization.
CLOSURE:
After completing the resective or disconnective part of the procedure, the surgical cavity is thoroughly irrigated in order to remove small blood clots and debris. The bone flap is secured back in its position by mini-plates and screws or by silk sutures. The surgical wound is closed in anatomical layers.
COMPLICATIONS:
Occasionally, some complications may occur including the need for a blood transfusion, aseptic meningitis, postoperative fevers and infection. Hydrocephalus (excess brain and spinal fluid in the brain) is condition that can occur either immediately after surgery or years later. This is very effectively treated through placement of a shunt.
- Brotis, A. G. (2015). Hemispherectomy: Indications, Surgical Techniques, Complications, and Outcome. Journal of Neurology & Neurophysiology, 06(04). https://doi.org/10.4172/2155-9562.1000300
- A case of Rasmussen’s Encephalitis | Pediatrics. (2021, October 23). [Video]. YouTube. https://www.youtube.com/watch?v=U2KXmakNh3w&t=368s
- E. (2016, August 18). Six Surgical Miracles. America College of Surgeons - Ohio. https://ohiofacs.org/six-surgical-miracles/
- Hemispherectomy - Epilepsy Treatment - UCLA Health Pediatric Neurosurgery, Los Angeles, CA. (n.d.). UCLA Health. https://www.uclahealth.org/mattel/pediatric-neurosurgery/hemispherectomy#:%7E:text=A%20hemispherectomy%20is%20a%20radical,seizures%20in%20carefully%20selected%20patients.
- Koch, D. (2021, May 21). A Medical Miracle: 12 Years After Half Of Her Brain Was Removed, Jessie Hall Shares How It Inspired Her To Help Others. Baltimore.Cbslocal.Com. https://baltimore.cbslocal.com/2021/05/20/jessie-hall-medical-miracle-half-brain-removed-johns-hopkins/
- [Rasmussen’s Encephalitis]. (n.d.). https://images.pexels.com/photos/6249932/pexels-photo-6249932.jpeg?auto=compress&cs=tinysrgb&dpr=2&w=500
- Rasmussen’s encephalitis. (2017, July 5). The Encephalitis Society. https://www.encephalitis.info/rasmussens-encephalitis#:%7E:text=Rasmussen%20encephalitis%20(RE)%2C%20also,%2Dyears%2Dold%20children).
- Symptoms of rasmussen’s encephalitis. (n.d.). [Photograph]. https://www.verywellhealth.com/thmb/q_hEeC7xUomNq6NjgNo6uGG8FuQ=/614x0/filters:no_upscale():max_bytes(150000):strip_icc():format(webp)/rasmussen-s-syndrome-and-rasmussen-s-encephalitis-4138156-01-164e4ba1640a4ae68f17d515b6648cf6.png
- Transparent high-resolution EEG array. (n.d.). [Photograph]. https://www.drugtargetreview.com/wp-content/uploads/brain-connectivity-e1536311594713.jpg
- Young, C. C., Williams, J. R., Feroze, A. H., McGrath, M., Ravanpay, A. C., Ellenbogen, R. G., Ojemann, J. G., & Hauptman, J. S. (2020). Pediatric functional hemispherectomy: operative techniques and complication avoidance. Neurosurgical Focus, 48(4), E9. https://doi.org/10.3171/2020.1.focus19889








Comments
Post a Comment